There’s a traditional story of obesity that goes something like this:
Obesity is a condition in which an organism has an excessive amount of fat. The definition of “excessive” is really only carefully defined in humans, in which excessive is defined as the ratio of the person’s weight (kg)/ the square of that person’s height (m) being over 30 (a.k.a. the body mass index, or BMI). This is defined as excessive because at or above that ratio, people tend to get negative health issues from all their fat, such as type 2 diabetes or cardiovascular disease.
Obesity is ultimately caused by an excess number of calories consumed vs. calories utilized by exercise and daily living. However, there are many factors that influence this, including diet, genetics, hormones, pollutants, and mental disorders.
Permanently losing weight as an obese person is very difficult. Some of the most effective weight loss interventions are surgeries that restrict the amount of food obese people can consume, and, more recently, medications that make people want to eat less.
Biologically, obesity is closely tied to a few different systems, especially the insulin system, which impacts the downstream blood lipid system, which includes fatty acids, cholesterol, and triglycerides. Obesity can cause malfunctions in both systems. In the insulin system, obesity causes type 2 diabetes, resulting in low levels of insulin in the blood and insulin resistance in the cells. In the blood lipid system, obesity generally results in inappropriately high levels of cholesterol and triglycerides. Malfunctions in both systems can also impact obesity or weight more generally.
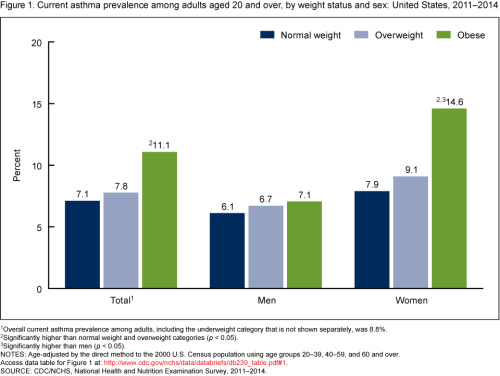
Obesity also impacts and can be impacted by a number of different biological systems, including the immune system and the endocrine system. Those connections are more obscure and not at play in all people. But, obesity does increase the risk of autoimmune disorders, especially in women, and it does increase the risk of endocrine disorders, also especially in women. Some autoimmune disorders, like lupus, can cause weight gain, as can some immunosuppressants. Some endocrine disorders can also cause weight gain.
This story is fine if you’re a primary care physician or someone writing an intro to a study. But it doesn’t really capture how weird obesity and weight in general is. As a result, it misses a lot of the complexity that actually matters if we want a scientific understanding of obesity.
Let’s start at the top, with the definition of obesity. As I mentioned, the standard definition of obesity is at or above a BMI of 30, because that value tends to be associated with negative health consequences in the people who are usually studied in obesity studies (i.e. white, middle-class Westerners). But the threshold value for negative health consequences from too much fat is not a constant. It changes depending on ethnic group. Aboriginal Australians tend to start experiencing health consequences at significantly lower BMIs than 30, Asian people tend to start experiencing negative health consequences at somewhat lower BMIs, and Inuits tend to start experiencing negative health consequences at higher BMIs.
Then, when we move onto the animal kingdom, for some species being obese isn’t associated with any negative health consequences at all. Not only are there obvious examples of fat animals like whales or seals, but pretty much all migratory and hibernatory animals put on an enormous amount of fat in preparation for their metabolically challenging migrations or hibernations. Needless to say, neither hummingbirds nor grizzly bears get heart attacks when they double their weight.
This switch from obesity being bad to obesity being good seems easy to trigger, too, if cavefish are any indication. As I wrote about previously, there are a couple different species of fish who live normal, fishy lives in streams near caves. However, if you raise them in complete darkness for a couple generations, they become obese, eyeless, and exceptionally long lived.
Now, if we keep moving down our standard story of obesity, we get the issue of obesity being all about a surplus of calories for an extended period of time, and weight loss being about a deficit of calories for an extended period of time. This ignores the complexity of how surpluses and deficits are “calculated”. When obese people lose a lot of weight, their body tries to get back to their old weight, with one study reporting that a formerly obese person had to eat only 800 calories per day to stop himself from gaining weight. Similarly, anorexic people are often “hypermetabolic” when they attempt to gain weight and no longer be anorexic, and are forced to eat enormous quantities to gain any weight at all.
And while the effective surgical interventions are straightforward enough to understand, the most recent, most effective medical interventions are anything but, as my last post was about. We thought the medical weight loss interventions were all about “making us feel like we’re full” by imitating the GLP-1 peptide released after eating, but, unfortunately, it’s way more complicated than that. For some reason, imitating that peptide or its complement, GIP, or imitating the inverse of that peptide or the inverse of its complement (i.e. the antagonists of those receptors) can all have surprisingly similar effects on both weight loss and/or protection from weight gain.
Convinced yet that this traditional story has holes? No? Well, let’s keep going. It’s true that obesity tends to lead to type 2 diabetes, which leads to underproduction of insulin and insulin resistance. However, directly administering insulin tends to lead to weight gain. Also, insulin resistance goes away almost immediately upon any amount of weight loss, and then re-establishes itself on any amount of weight gain. However, both fat cell creation (lipogenesis) and fat cell destruction (lipolysis) also lead to drops in insulin resistance. Oh, and also, pretty much any medication that interacts with GLP-1 receptors or GIP receptors, whether agonizing them or antagonizing them, leads to insulin secretion.
Then, last, when it comes to obesity, autoimmune, and endocrine disorders, well, as I mentioned, a lot of those only affect women, like obesity-associated asthma. Now, while it’s true that autoimmune and endocrine disorders disproportionately impact women, still, there’s no theory of obesity that explains why some of those would only impact women. The normal explanations, like fat cells causing inflammation, don’t cut it.
Towards a new theory of obesity
Imagine you’re a gardener harvesting blackberries at the end of summer. You’re faced with a basic issue: what do you do with the blackberries you harvest?
Well, obviously, you’re going to save some for now, some for later, and some for way later. Maybe you’ll eat some of the blackberries, put some in a basket, freeze some, and turn the rest into a preserve. And these are going to be your options, generally speaking, no matter who you are or where you are growing blackberries. There are only so many options on what you can do with blackberries.
What is dependent on who (or where) you are, however, is how you allocate your blackberries. If you haven’t eaten breakfast yet, maybe you’ll eat a lot of blackberries now, but you won’t want any for dinner. If your family loves blackberries, maybe you’ll save a ton of blackberries for dinner tonight. If the local supermarket never stocks blackberries, maybe you’ll want to freeze a lot. As a result of this, it’s impossible for me to make a generalization about the best way for you to handle your blackberries without knowing more about your situation.
That’s not to say I can never make a judgment about whether you’ve handled your blackberries the right way. I have an uncle who used to sneak jars of applesauce into our pantry whenever he’d visit, because his apple trees would produce too many apples for his family alone to consume, and he didn’t have the time or inclination to sell them. His options were to let the apples rot in his yard or to reverse steal applesauce from (to?) us. Uncle Cary did not handle his apples the right way, and, if he had grown blackberries, would probably have not handled his blackberries the right way either.
But, a priori, a snapshot of anyone’s blackberry (or apple) plans or larder doesn’t let us know if they are handling their blackberries correctly. Even Uncle Cary’s basement, overflowing with applesauce (and pickles, and canned peaches, and tomato sauce), wouldn’t necessarily have tipped us off. After all, he could have just been storing them temporarily while he waited to donate them to whatever soup kitchen he hadn’t already overloaded with stuff.
So, having a basement overflowing with blackberry preserves might mean that you’re bad at planning, and soon you’ll need to reverse-steal your preserves away. Or it might mean that you’re stocked up for the winter because you don’t want to buy any blackberry preserve. Or it might mean that you got way more blackberries than you expected, or that you actually couldn’t freeze as many blackberries as expected, or any number of other issues.
Obesity, in this case, is a lot like blackberries. If there is some sort of bodily compensation for the fat, and the bodily compensation is negatively impacting overall health, then we can say the excess fat is bad, just like we can say my Uncle Cary grew too many apples because he was forced to hide them in our pantry, annoying my mom. But then we need to identify what the compensation is, how it functions to alleviate whatever the stresses of obesity are, and what the negative health consequences are.
I understand that this makes it way more difficult to make broad statements about obesity because I’ve taken away an easy definition. However, this reframing is beneficial for three main reasons:
1. It guarantees that we’re only talking about obesity as an actual disease or condition (i.e. something that negatively impacts health), rather than the state of weighing more than an arbitrary cut off.
2. It allows for clear, unambiguous animal models of obesity, rather than having to come up with reasons as to why bears having a lot of fat is good, but dogs having a lot of fat is bad.
3. It separates out bodily compensations for fat from the negative health consequences of those bodily compensations. Right now, those are mixed up, so insulin resistance, which, if we’re judging by animal models (and the way GLP-1 receptor agonists work), is probably compensating for some effect of obesity, is considered a negative health consequence of obesity instead.
This would also make it much easier to predict the course of obesity and the effect of interventions. Right now, if you tell me someone is obese, I can’t even tell you what their weight will be in a year, if, for example, they’re a bodybuilder on a bulk cycle. And I definitely can’t tell you with certainty if they will develop any other conditions or negative health problems.
However, if someone has obesity-related type 2 diabetes? Well, if they don’t do anything, that will continue and get worse, with their pancreatic beta cells dying out and producing less and less insulin. After all, obesity-related type 2 diabetes doesn’t spontaneously remit, and it wouldn’t develop in a bodybuilder who’s bulking. If that person then gets a gastric bypass, though, they will almost certainly start to lose weight, and their type 2 diabetes will go into remission.
We can then start talking about just being fat, or even extremely fat, not as a health condition but as a state of being that’s determined by bodily processes. While the cardiovascular system of a very fat person probably doesn’t look like the cardiovascular system of a very fat hummingbird preparing for migration, the way that they store and maintain fat does have a lot of similarities, especially with the connections to the insulin system.
This can be put in a useful contrast to the way that young individuals, both human and otherwise, find it impossible to put on weight. My brothers and I used to eat 2000+ calories at fast food restaurants just for fun in eating competitions without putting on a single pound. Why were we able to do that? I don’t know, but we won’t be able to find out with the way we’re thinking about obesity right now.
Energy acquisition, metabolism, and storage is a fundamental biological problem. Fat storage is a crucial part of every animal’s solution to this problem. But, because we insist on thinking of being fat as a human health issue, rather than a method that basically the entire animal kingdom has adopted to solve the energy storage problem, we have failed to understand fatness in either its biological form or, ironically, even as a health issue.
Every drug developer knows the acronym ADME: absorption, deposition, metabolism, excretion. It’s the way of describing what happens to any drug that enters the body, and every drug that gets approved gets characterized in those terms. We should be able to do the same thing for food and understand the path of food in at least as much detail. But we’re not there yet.